Rickettsia rickettsii
| Rickettsia rickettsii | |
|---|---|
| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Alphaproteobacteria |
| Order: | Rickettsiales |
| Family: | Rickettsiaceae |
| Genus: | Rickettsia |
| Species group: | Spotted fever group |
| Species: | R. rickettsii
|
| Binomial name | |
| Rickettsia rickettsii Brumpt, 1922
| |
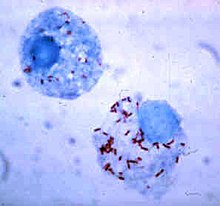
Rickettsia rickettsii is a Gram-negative, intracellular, coccobacillus bacterium that was first discovered in 1902.[1] Having a reduced genome, the bacterium harvests nutrients from its host cell to carry out respiration, making it an organoheterotroph. Maintenance of its genome is carried out through vertical gene transfer where specialization of the bacterium allows it to shuttle host sugars directly into its TCA cycle.[2]
Other characteristics of the bacteria include membrane proteins that are useful in the identification of R. rickettsii strains and useful in the targeting of antibiotics. A capsule encircling the bacterium allows for attachment to host cells and additionally acts as a defense mechanism for resisting phagocytosis. Varying strains of R. rickettsii have different genotypes and phenotypes that alter the pathogenicity, virulence, and appearance of the bacteria.[3][4][5]
R. rickettsii is the causative agent of Rocky Mountain Spotted Fever and is transferred to its host via a tick bite. It is one of the most pathogenic Rickettsia species[6] and affects a large majority of the Western Hemisphere, most commonly the Americas.[7] The pathogenic agent has been found on every continent, except Antarctica; however, Rocky Mountain Spotted Fever occurs mostly in North, Central, and South America.[7] This prevalence is due to R. rickettsi thriving in warm, damp environments.[8] These environments provide sufficient conditions for the amplification of the bacteria within a vertebrate host, such as a horse or dog. The bacteria are transmitted through the vector, a tick, to a vertebrate host where it can then be amplified and passed on to a person, resulting in the zoonotic disease.[9]
Headache, high fever, and spotted rash are some effects of the disease with more severe cases resulting in organ damage and coma.[10][11][12] Antibiotics, such as doxycycline, target the ribosome of R. rickettsii in order to inhibit protein synthesis of the bacteria, providing a form of treatment for the disease.[13]
Transmission cycle
[edit]Ecology
[edit]
The most common hosts for R. rickettsii are ticks.[8] Ticks that carry R. rickettsii fall into the family of Ixodidae ticks, also known as "hard-bodied" ticks.[15] Ticks are vectors, reservoirs, and amplifiers of this bacteria.[8]
There are currently three known tick species that commonly carry R. rickettsii. The American Dog Tick (Dermacentor variabilis), mainly found in the eastern United States, is the most common vector for R. rickettsii. The Rocky Mountain Wood Tick (Dermacentor andersoni), found in the Rocky Mountain States, and the Brown Dog Tick (Rhipicephalus sanguineus), found in select areas of the southern United States, are also known vectors of the pathogen.[15][16] Ecology Infecting horses and capybaras, the cayenne tick turns vertebrate hosts into amplifier hosts of the bacteria. Other small rodent species serve as amplifier hosts in the United States and South America.[9]
Transmission in ticks
[edit]Ticks can contract R. rickettsii by many means. First, an uninfected tick can become infected when feeding on the blood of an infected vertebrate host; such as a rabbit, during the larval or nymph stages, this mode of transmission is called transstadial transmission.[17] Once a tick becomes infected with this pathogen, they are infected for life. Both the American Dog Tick and the Rocky Mountain Wood Tick serve as long-term reservoirs for Rickettsia rickettsii, in which the organism resides in the tick posterior diverticula of the midgut, the small intestine, and the ovaries.[17] In addition, an infected male tick can transmit the organism to an uninfected female during mating. However, this process is unlikely to play a major role in the maintenance of R. rickettsii within a population as females infected during mating have not been observed to produce infected offspring. Infected female ticks can transmit the infection to their offspring, in a process known as transovarian passage.[18] Notably, R. rickettsii is inefficient at infecting the ovaries of adult female ticks, resulting in a lowered rate of vertical transmission.[19] Rickettsial colonization of the ovaries sees higher success when ticks obtain the pathogen as a larva or nymph.[20] Reduced fecundity is also observed in ticks infected with R. rickettsii.[21] As a result of these limitations, long-term maintenance of R. rickettsii in populations of ticks relies mainly on horizontal transmission through the exchange of bacteria during feedings of infected hosts.[21][22]
The duration of tick attachment, bacterial loads in tick saliva, and the transmission efficiency of Rickettsia are important factors underlying transmission from ticks to humans.[23]
Transmission in mammals
[edit]Due to its confinement in the midgut and small intestine, Rickettsia rickettsii can be transmitted to mammals, including humans.
Transmission can occur in multiple ways. The most common way of contraction is by the bite of an infected tick. After getting bitten by an infected tick, R. rickettsiae is transmitted into the bloodstream by tick salivary secretions.[24] The saliva of ticks contain immunomodulatory agents which effect immune defenses in the host. This allows for R.rickettsiae to be transmitted with little to no resistance from the host's immune system.[24]Another way to contract the infection is through contact with an infected host's feces. If an infected host's feces come into contact with an open skin barrier, it is possible for the disease to be transmitted. An uninfected host can become infected when eating food that contains the feces of the infected vector.[24]
Having multiple modes of transmission ensures the persistence of R. rickettsii in a population. Additionally, having multiple modes of transmission helps the disease adapt better to new environments and prevents it from becoming eradicated. R. rickettsii has evolved a number of strategic mechanisms, or virulence factors, that allow it to invade the host immune system and successfully infect its host.[25]
Physiology
[edit]Metabolic Pathways
[edit]R. rickettsii are obligate intracellular bacteria, meaning they need a host cell in order to replicate and survive. In fact, no glycolytic enzymes for the breakdown of intact glucose remain in R. rickettsii's genome.[26] It is theorized that while R. rickettsii once possessed complete, complex metabolic pathways that allowed it to survive outside a host, evolutionary pressures caused progressive genomic reduction [27] that now limits metabolism to the tricarboxylic acid cycle (TCA).[26] Remnants of these lost metabolic pathways can be seen in analyses of R. rickettsii's genome, which contain some identified remnant enzymes of pathways that remain unfunctional in vivo.[27] This decrease in available metabolic pathways has left R. rickettsii largely dependant on a range of transport systems to harvest essential amino acids, nucleic acids, and other metabolites from its host.
The primary carbon source of R. rickettsii is pyruvate, though many other amino acids and TCA cycle intermediates such as glutamine, glutamate,[28] and malate can be used. For lipid metabolism, a complete map of fatty acid synthesis enzymes have been found, allowing R. rickettsii to construct a viable cell membrane with lipopolysaccharides (LPS). Regarding synthesis of a peptidoglycan layer, there is speculation as to whether key components are synthesized internally or imported and modified for use.[26] Pathways for producing critical small molecules such as riboflavin (B2), nicotinamide (B3), pantothenate (B5), pyridoxine (B6), and biotin (B7) are all missing key enzymes, forcing R. rickettsii to rely solely on transmembrane transport proteins.[26]
Overall, R. rickettsii has a genome that does not encode many of the enzymes and proteins that are required for several pathways besides the TCA cycle. These bacteria import many of the intermediates, cofactors, and byproducts from the host cells' metabolic pathways to use for their own benefit and synthesis of necessary structures and energy for survival.[2]
Morphology
[edit]R. rickettsii has many vital proteins within its cellular membranes. One of these proteins is YbgF, which maintains the structure of the cellular membrane. YbgF is found within both the inner and outer membranes along with another protein called TolC. TolC is a transport protein that connects to other transport proteins within the periplasmic space and inner membrane. These two proteins are believed to be associated with pathogenicity of this microbe and serve as specific points that antibodies can bind to in order to prevent the bacteria from interacting with host cells.[3]
R. rickettsii has an outer layer or a "microcapsule", in addition to the traditional peptidoglycan cell wall. The function of the microcapsule resembles that of slime layers, or S-layers, of other bacteria. This slime layer consists mostly of polysaccharides and is constantly undergoing changes in reaction to chemical or physiological events. Research to precisely determine the function of the slime layer is currently limited due to high risk of infection while working with this bacterium; however, scientists can infer based on conclusions from other studies that it is likely that this slime layer is used for antiphagocytic properties, which prevent phagocytes from engulfing and killing the R. rickettsii bacteria, and attachment to host cells in preparation to penetrate and infect those cells.[29]
Pathophysiology
[edit]While humans are hosts for R. rickettsii, they do not contribute to rickettsial transmission. Rather, the pathogen is maintained through its vector: ticks.[25] R. rickettsii invades the endothelial cells that line the blood vessels in the host's body. Increased permeability of vessels, microvascular hemorrhages, and necrosis can result from damage to the cells.[12] The pathogen causes changes in the host cell cytoskeleton that induces phagocytosis, and R. rickettsii replicates further and infects other cells in the host's body.[30] R. rickettsii's survival in immune system cells increases the pathogen's virulence in mammalian hosts.
Actin-Based Motility (ABM) is a virulence factor that allows for the pathogen to evade the host's immune cells and spread to neighboring cells. It is suggested that the Sca2 gene, which is an actin-polymerizing determinant, is a distinguishing factor for the Rickettsia family, as R. rickettsii mutants with a Sca2 transposon the bacteria can avoid autophagic processes by host phagocytic cells. This leads to an increase in disease manifestation for the host.[25]
R. rickettsii is also able to suppress immune responses while dwelling in infected cells by creating inhibitory proteins such as Rickettsial ankyrin repeat protein 2 (RARP2). RARP2 mediates the fragmentation of TGN, or the trans-Golgi network, causing attenuation of vesicular transport and glycosylation defects in infected host cells. There are two important proteins within the host cell that are affected by these glycosylation defects: TGN46 and major histocompatibility complex class 1 (MHC-I). MHC-I is an important protein for defending against pathogens as it functions as an antigen presenting complex signaling its infection status to lyphocytes. However, since RARP2 causes attenuation of vesicular transport, MHC-I is unable to be transported to the plasma membrane and the infected cell will not be able to alert host immune cells. Thus, the bacterial cells are able to avoid certain immune responses and allow for proliferation within a host cell.[31]
Genome and phenotypes
[edit]R. rickettsii is an obligate intracellular alpha proteobacterium that belongs to the Rickettsiacea family.[6] It has a genome that consists of about 1.27 Mbp with ~1,350 predicted genes,[4] which is smaller compared to most other bacteria. This small genome size allows the bacteria to maintain an intracellular lifestyle with increased pathogenicity from gene reduction.[32] It is maintained in its tick host by transovarial transmission.[6] The multiplication of R. rickettsii is by binary fission inside the cytosol.[1]
Genomic comparison of strains
[edit]R. rickettsii has a relatively small genome; however, variances in gene expression between different strains can lead to various functions of the bacteria. For instance, there are two major strains of R. rickettsii called the Iowa and the Sheila Smith strains. The Sheila Smith strain is a virulent strain, while the Iowa strain is an avirulent strain. Microarrays revealed that there were only four distinct differences in the gene expression of R. rickettsii; however, these four changes lead to complete differences in virulence, and thus the niche of the bacteria.[33] A key feature allowing for differentiation is the rickettsial outer membrane protein, rOmpA and rOmpB [4] which contributes to the identification of R. rickettsii strains as virulent. The detection of single nucleotide polymorphisms (SNPs) are used to differentiate these strains.[4]
Clinical manifestations
[edit]The Centers for Disease Control and Prevention states that the diagnosis of Rocky Mountain Spotted Fever (RMSF) must be made based on the clinical signs and symptoms of the patient and then later be confirmed using specialized laboratory tests. However, the diagnosis of Rocky Mountain Spotted Fever is often misdiagnosed due to its non-specific onset. The majority of infections from R. rickettsii occur during the warmer months between April and September. Symptoms can take 1–2 days to 2 weeks to present themselves within the host.[10] The diagnosis of RMSF is easier when there is a known history of a tick bite or if the rash is already apparent in the affected individual.[34] If not treated properly, the illness may become serious, leading to hospitalization and possible fatality.[35]
Signs and symptoms
[edit]During the initial stages of the disease, the infected person may experience headaches, muscle aches, chills, and high fever. Other early symptoms may include nausea, vomiting, loss of appetite, and conjunctival injection (red eyes). Most people infected by R. rickettsii develop a spotted rash, that begins to appear 2 to 4 days after the individual develops a fever. If left untreated, more severe symptoms may develop; these symptoms may include insomnia, compromised mental ability, coma, and damage to the heart, kidneys, liver, lungs, or additional organs.[11][10]

The classic Rocky Mountain Spotted Fever rash occurs in about 90% of patients and develops 2 to 5 days after the onset of fever. The rash can differ greatly in appearance along the progress of the R. rickettsii infection.[11] It is not itchy and starts out as flat pink macules located on the affected individual's hands, feet, arms, and legs.[34] During the course of the disease, the rash may form petechiae and take on a more darkened reddish purple spotted appearance, signifying severe disease.[36]
In rarer cases, patients may present with chest pain due to myocarditis. Additionally, rare symptoms include vision impairment and arthritis that may exist as chronic sequelae, lasting anywhere from 10 days to 4 years. Other chronic sequelae include some cases of neurological challenges, such as impaired speech, dysphagia, ataxia, memory loss, cortical blindness, and decreased attention span. Necrosis of skin is another rare case of sequelae.[16][37]
Severe infections
[edit]Patients with severe infections may require hospitalization. The more severe symptoms occur later in response to thrombosis (blood clotting) caused by R. rickettsii targeting endothelial cells in vascular tissue.[10][38] One manifestation of this damage is the development of a petechial rash, which in 60% of cases presents within 6 days of initial symptoms. Petechial rashes are indicative of more severe disease progression.[39] Patients may become hyponatremic, experience elevated liver enzymes, and other more pronounced symptoms. It is not uncommon for severe cases to involve respiratory system, central nervous system, gastrointestinal system, or renal system complications. In the case of meningoencephalitis, R. rickettsii causes cellular damage to brain tissue, resulting in inflammation. Additionally, acute respiratory distress syndrome and Coagulopathy occur in cases that advance to severe stages of RMSF.[12] This disease is worst for elderly patients, males, African Americans, alcoholics, and patients with G6PD deficiency. The mortality rate for RMSF is 3 to 5 percent in treated cases, but 13 to 25 in untreated cases.[34] Deaths usually are caused by heart and kidney failure.[18]
Treatment
[edit]RMSF symptoms can vary from moderate to severe cases, and a delay in treatment is often associated with a higher case-fatality rate.[40] The most common and effective treatment for Rocky mountain spotted fever is the anti-microbial agent doxycycline.[41] This antibiotic acts as a bacteriostatic drug by inhibiting protein synthesis via blockage of the 30S ribosomal subunit.[13]
Other treatments with chloramphenicol, fluoroquinolones, and macrolides have been explored. However, treatment with only chloramphenicol compared to other treatments (tetracycline-class drugs only, both chloramphenicol and tetracycline-class drugs, and neither drug) was associated with a case-fatality rate three times higher.[40] Chloramphenicol, like doxycycline, also functions as a bacteriostatic drug, but it binds to the 50S ribosomal subunit in order to prevent protein synthesis. Macrolides target the 50S subunit as well; however, they block the exit site for peptides, while chloramphenicol blocks the aminoacyl-tRNA attachment site for transfer RNA.[42]
History
[edit]The first documented case of Rocky Mountain Spotted Fever (RMSF) presented in the Boise, Idaho in 1896 after being recognized by Major Marshall H. Wood.[43] At the time of discovery, not much information was known about the disease. It was originally called "Black Measles" due to the infected area turning black during the late stages of the disease.[44] The first clinical description of Rocky Mountain Spotted Fever was reported in Snake River Valley in 1899 by Edward E. Maxey.[45] At the time, 69% of individuals diagnosed with RMSF died.[43] It was theorized that the wood tick played a critical role as a vector of disease, based on apparent correlation between tick exposure and disease, as well as the geographic and seasonal presentation. [46]
Howard Ricketts (1871–1910), an associate professor of pathology at the University of Chicago in 1902, was the first to identify and study R. rickettsii on a microbial level.[43] His research consisted of interviewing victims of the disease, as well as collecting infected animals to study. He was also known to inject himself with pathogens to more accurately document their effects. Ricketts was the first to identify the pathogen responsible for RMSF as a gram negative bacillus bacteria, and confirm a route of transmission from infected ticks in a guinea pig model. [46] His research provided valuable information on the organism's vector and route of transmission.[43]
Simeon Burt Wolbach is credited for the first detailed, published description of the pathogenic agent that causes R. rickettsii in 1919. Wolbach described RMSF using the process of Giemsa staining,[43] and positively identified the bacterium as frequently residing within endothelial cells.[47][46]
The once lethal infection RMSF has become curable due to the modern availability of antibiotics. Broad spectrum antibiotics chloramphenicol and tetracycline-class drugs, like doxycycline, were first harnessed as treatment for RMSF in the late 1940s.[46] Before their discovery, 1 in 5 infected patients died.[48] Treatment recommendations changed in the 1990s to support primary therapeutic use of tetracycline-class drugs, and the current recommended treatment reflects this, as doxycycline is most commonly prescribed.[41] This change in treatment recommendation coincided with a decrease in annual case-fatality rates (CFRs) from the 1980s on to the early 1990s.[49] Since then, the fatality rate has dropped to between 5 and 10%.[49]
References
[edit]- ^ a b Patel S, Pedroza LV (2023-06-13). Bronze MS (ed.). "Rocky Mountain Spotted Fever (RMSF): Background, Etiology and Pathophysiology, Epidemiology". Medcape.
- ^ a b Driscoll TP, Verhoeve VI, Guillotte ML, Lehman SS, Rennoll SA, Beier-Sexton M, et al. (September 2017). "Wholly Rickettsia! Reconstructed Metabolic Profile of the Quintessential Bacterial Parasite of Eukaryotic Cells". mBio. 8 (5): e00859–17. doi:10.1128/mBio.00859-17. PMC 5615194. PMID 28951473.
- ^ a b Gong W, Qi Y, Xiong X, Jiao J, Duan C, Wen B (2015-03-04). "Rickettsia rickettsii outer membrane protein YbgF induces protective immunity in C3H/HeN mice". Human Vaccines & Immunotherapeutics. 11 (3): 642–9. doi:10.1080/21645515.2015.1011572. PMC 4514262. PMID 25714655.
- ^ a b c d Clark TR, Noriea NF, Bublitz DC, Ellison DW, Martens C, Lutter EI, et al. (April 2015). Morrison RP (ed.). "Comparative genome sequencing of Rickettsia rickettsii strains that differ in virulence". Infection and Immunity. 83 (4): 1568–76. doi:10.1128/IAI.03140-14. PMC 4363411. PMID 25644009.
- ^ Clark TR, Ellison DW, Kleba B, Hackstadt T (April 2011). Morrison RP (ed.). "Complementation of Rickettsia rickettsii RelA/SpoT restores a nonlytic plaque phenotype". Infection and Immunity. 79 (4): 1631–7. doi:10.1128/IAI.00048-11. PMC 3067566. PMID 21300770.
- ^ a b c Hackstadt T. "Biology of Rickettsia".
- ^ a b Conover MR, Vail RM (2014). "Rocky Mountain Spotted Fever and Other Spotted Fevers". Human Diseases from Wildlife. CRC Press. pp. 252–265. doi:10.1201/b17428-18. ISBN 978-0-429-10009-3. Retrieved 2023-10-31.
- ^ a b c Parola P, Paddock CD, Raoult D (October 2005). "Tick-borne rickettsioses around the world: emerging diseases challenging old concepts". Clinical Microbiology Reviews. 18 (4): 719–756. doi:10.1128/CMR.18.4.719-756.2005. PMC 1265907. PMID 16223955.
- ^ a b Labruna MB (May 2009). "Ecology of rickettsia in South America". Annals of the New York Academy of Sciences. 1166 (1): 156–166. Bibcode:2009NYASA1166..156L. doi:10.1111/j.1749-6632.2009.04516.x. PMID 19538276.
- ^ a b c d "Rocky Mountain Spotted Fever". Red Book. American Academy of Pediatrics. 2018-05-01. pp. 697–700. doi:10.1542/9781610021470-part03-rocky_mountain. ISBN 978-1-61002-147-0. S2CID 232564979. Retrieved 2023-10-21.
- ^ a b c "Rocky Mountain spotted fever home". Centers for Disease Control and Prevention (CDC). 2019-05-07. Retrieved 2023-10-21.
- ^ a b c Drexler N (2020). "Persistent Sequelae of Rocky Mountain Spotted Fever: Clinical Evidence, Cost, and Public Health Implications for Arizona Tribal Communities". ProQuest. ProQuest 2410817332. Retrieved February 29, 2024.
- ^ a b Holmes NE, Charles PG (January 2009). "Safety and Efficacy Review of Doxycycline". Clinical Medicine. Therapeutics. 1: CMT.S2035. doi:10.4137/CMT.S2035. ISSN 1179-1713.
- ^ "Ixodes species". Learn About Parasites. Western College of Veterinary Medicine. Retrieved 2023-10-26.
- ^ a b Parola P, Davoust B, Raoult D (2005-06-01). "Tick- and flea-borne rickettsial emerging zoonoses". Veterinary Research. 36 (3): 469–492. doi:10.1051/vetres:2005004. PMC 7996843. PMID 15845235.
- ^ a b Jay R, Armstrong PA (2020). "Clinical characteristics of Rocky Mountain spotted fever in the United States: A literature review". Journal of Vector Borne Diseases. 57 (2): 114–120. doi:10.4103/0972-9062.310863. PMID 34290155.
- ^ a b Ravindran R, Hembram PK, Kumar GS, Kumar KG, Deepa CK, Varghese A (March 2023). "Transovarial transmission of pathogenic protozoa and rickettsial organisms in ticks". Parasitology Research. 122 (3): 691–704. doi:10.1007/s00436-023-07792-9. PMC 9936132. PMID 36797442.
- ^ a b Tortora GJ, Funke BR, Case CL (2013). Microbiology: An Introduction. United States of America: Pearson Education, Inc. pp. 661–2. ISBN 978-0-321-73360-3.
- ^ Burgdorfer W, Brinton LP (November 1975). "Mechanisms of transovarial infection of spotted fever Rickettsiae in ticks". Annals of the New York Academy of Sciences. 266 (1): 61–72. Bibcode:1975NYASA.266...61B. doi:10.1111/j.1749-6632.1975.tb35088.x. PMID 829476.
- ^ Piranda EM, Faccini JL, Pinter A, Pacheco RC, Cançado PH, Labruna MB (January 2011). "Experimental infection of Rhipicephalus sanguineus ticks with the bacterium Rickettsia rickettsii, using experimentally infected dogs". Vector Borne and Zoonotic Diseases. 11 (1): 29–36. doi:10.1089/vbz.2009.0250. PMID 20569011.
- ^ a b Laukaitis HJ, Macaluso KR (August 2021). "Unpacking the intricacies of Rickettsia-vector interactions". Trends in Parasitology. 37 (8): 734–746. doi:10.1016/j.pt.2021.05.008. PMC 8344978. PMID 34162522.
- ^ Levin ML, Zemtsova GE, Killmaster LF, Snellgrove A, Schumacher LB (June 2017). "Vector competence of Amblyomma americanum (Acari: Ixodidae) for Rickettsia rickettsii". Ticks and Tick-Borne Diseases. 8 (4): 615–622. doi:10.1016/j.ttbdis.2017.04.006. PMC 5657001. PMID 28433728.
- ^ Kim HK (September 2022). "Rickettsia-Host-Tick Interactions: Knowledge Advances and Gaps". Infection and Immunity. 90 (9): e0062121. doi:10.1128/iai.00621-21. PMC 9476906. PMID 35993770.
- ^ a b c Kim HK (September 2022). "Rickettsia-Host-Tick Interactions: Knowledge Advances and Gaps". Infection and Immunity. 90 (9): e0062121. doi:10.1128/iai.00621-21. PMC 9476906. PMID 35993770.
- ^ a b c Helminiak L, Mishra S, Kim HK (December 2022). "Pathogenicity and virulence of Rickettsia". Virulence. 13 (1): 1752–71. doi:10.1080/21505594.2022.2132047. PMC 9553169. PMID 36208040.
- ^ a b c d Fuxelius HH, Darby A, Min CK, Cho NH, Andersson SG (December 2007). "The genomic and metabolic diversity of Rickettsia". Res Microbiol. 158 (10): 745–53. doi:10.1016/j.resmic.2007.09.008. PMID 18031998.
- ^ a b Blanc G, Ogata H, Robert C, Audic S, Suhre K, Vestris G, et al. (January 2007). "Reductive genome evolution from the mother of Rickettsia". PLoS Genet. 3 (1): e14. doi:10.1371/journal.pgen.0030014. PMC 1779305. PMID 17238289.
- ^ Rees HB, Weiss E (February 1968). "Glutamate catabolism of Rickettsia rickettsi and factors affecting retention of metabolic activity". J Bacteriol. 95 (2): 389–96. doi:10.1128/jb.95.2.389-396.1968. PMC 252031. PMID 5640379.
- ^ Silverman DJ, Wisseman CL, Waddell AD, Jones M (October 1978). "External layers of Rickettsia prowazekii and Rickettsia rickettsii: occurrence of a slime layer". Infect Immun. 22 (1): 233–46. doi:10.1128/iai.22.1.233-246.1978. PMC 422141. PMID 83297.
- ^ Sahni A, Fang R, Sahni SK, Walker DH (January 2019). "Pathogenesis of Rickettsial Diseases: Pathogenic and Immune Mechanisms of an Endotheliotropic Infection". Annual Review of Pathology. 14: 127–152. doi:10.1146/annurev-pathmechdis-012418-012800. PMC 6505701. PMID 30148688.
- ^ Kellermann M, Scharte F, Hensel M (June 2021). "Manipulation of Host Cell Organelles by Intracellular Pathogens". International Journal of Molecular Sciences. 22 (12): 6484. doi:10.3390/ijms22126484. PMC 8235465. PMID 34204285.
- ^ Merhej V, Angelakis E, Socolovschi C, Raoult D (July 2014). "Genotyping, evolution and epidemiological findings of Rickettsia species". Infection, Genetics and Evolution. 25: 122–137. Bibcode:2014InfGE..25..122M. doi:10.1016/j.meegid.2014.03.014. PMID 24662440.
- ^ Ellison DW, Clark TR, Sturdevant DE, Virtaneva K, Porcella SF, Hackstadt T (February 2008). "Genomic comparison of virulent Rickettsia rickettsii Sheila Smith and avirulent Rickettsia rickettsii Iowa". Infection and Immunity. 76 (2): 542–550. doi:10.1128/IAI.00952-07. PMC 2223442. PMID 18025092.
- ^ a b c Palatucci OA, Marangoni BA. "Rocky Mountain Spotted Fever". SpringerReference. Berlin/Heidelberg: Springer-Verlag. Archived from the original on 6 May 2020. Retrieved 2023-10-21.
- ^ "Rocky Mountain Spotted Fever". www.hopkinsmedicine.org. 2019-11-19. Retrieved 2023-11-03.
- ^ "Signs and symptoms of RMSF for healthcare providers". Centers for Disease Control and Prevention (CDC). 2019-02-19. Retrieved 2023-11-03.
- ^ Doyle A, Bhalla KS, Jones JM, Ennis DM (October 2006). "Myocardial involvement in rocky mountain spotted fever: a case report and review". The American Journal of the Medical Sciences. 332 (4): 208–210. doi:10.1097/00000441-200610000-00009. PMID 17031247.
- ^ Kristof MN, Allen PE, Yutzy LD, Thibodaux B, Paddock CD, Martinez JJ (February 2021). "Significant Growth by Rickettsia Species within Human Macrophage-Like Cells Is a Phenotype Correlated with the Ability to Cause Disease in Mammals". Pathogens. 10 (2): 228. doi:10.3390/pathogens10020228. PMC 7934685. PMID 33669499.
- ^ Phillips J (January 2017). "Rocky Mountain Spotted Fever". Workplace Health & Safety. 65 (1): 48. doi:10.1177/2165079916683711. PMID 28055518.
- ^ a b Botelho-Nevers E, Raoult D (October 2011). "Host, pathogen and treatment-related prognostic factors in rickettsioses". European Journal of Clinical Microbiology & Infectious Diseases. 30 (10): 1139–50. doi:10.1007/s10096-011-1208-z. PMID 21519943.
- ^ a b Breitschwerdt EB, Papich MG, Hegarty BC, Gilger B, Hancock SI, Davidson MG (April 1999). "Efficacy of doxycycline, azithromycin, or trovafloxacin for treatment of experimental Rocky Mountain spotted fever in dogs". Antimicrobial Agents and Chemotherapy. 43 (4): 813–821. doi:10.1128/AAC.43.4.813. PMC 89211. PMID 10103185.
- ^ Oong GC, Tadi P (2024). Chloramphenicol. StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32310426. NBK555966. Retrieved 2024-04-10.
- ^ a b c d e Patel S, Pedroza LV (2023-06-13). Bronze MS (ed.). "Rocky Mountain Spotted Fever (RMSF): Background, Etiology and Pathophysiology, Epidemiology". Medcape.
- ^ "Rocky Mountain Spotted Fever". www.niaid.nih.gov. 2014-07-08. Retrieved 2023-10-31.
- ^ Xiao Y, Beare PA, Best SM, Morens DM, Bloom ME, Taubenberger JK (March 2023). "Genetic sequencing of a 1944 Rocky Mountain spotted fever vaccine". Scientific Reports. 13 (1): 4687. Bibcode:2023NatSR..13.4687X. doi:10.1038/s41598-023-31894-0. PMC 10031714. PMID 36949107.
- ^ a b c d Thorner AR, Walker D, Petri W (1998). "Rocky Mountain Spotted Fever". Clinical Infectious Diseases. 27 (6): 1353–59. doi:10.1086/515037. JSTOR 4481728. PMID 9868640.
- ^ Conover MR, Vail RM (2014). "Rocky Mountain Spotted Fever and Other Spotted Fevers". Human Diseases from Wildlife. CRC Press. pp. 252–265. doi:10.1201/b17428-18. ISBN 978-0-429-10009-3. Retrieved 2023-10-31.
- ^ Holman RC, Paddock CD, Curns AT, Krebs JW, McQuiston JH, Childs JE (December 2001). "Analysis of risk factors for fatal Rocky Mountain Spotted Fever: evidence for superiority of tetracyclines for therapy". The Journal of Infectious Diseases. 184 (11): 1437–44. doi:10.1086/324372. PMID 11709786.
- ^ a b "Epidemiology and statistics of spotted fever rickettsioses". Centers for Disease Control and Prevention (CDC). 2022-08-15. Retrieved 2023-10-31.
Further reading
[edit]- Dumbler SJ, Walker DH (2006). "Order II. Rickettsiales Gieszczkiewicz 1939..". In Garrity G, Brenner DJ, Staley JT, Krieg NR, Boone DR, Vos PD, et al. (eds.). The Proteobacteria (Part C). Bergey's Manual® of Systematic Bacteriology. Vol. 2. Springer. pp. 96–. ISBN 978-0-387-29298-4.
- Todar K (2008–2012). "Rickettsial Diseases, including Typhus and Rocky Mountain Spotted Fever". Todar's Online Textbook of Bacteriology.
- Walker DH, ed. (1988). Biology of Rickettsial Diseases. Boca Raton, Florida: CRC Press. ISBN 978-0-8493-4382-7. OCLC 16832977.
- Weiss K. The Role of Rickettsioses in History. pp. 2–14.
- Weiss E. History of Rickettsiology. pp. 15–32.
- Wilson BA, Salyers AA, Whitt DD, Winkler ME (2011). Bacterial Pathogenesis: A Molecular Approach (3rd ed.). American Society for Microbiology. ISBN 978-1-55581-418-2. OCLC 710835671.
External links
[edit]- "Rickettsia rickettsii genomes and related information". PATRIC, Bioinformatics Resource Center. NIAID. Archived from the original on 2014-03-07. Retrieved 2010-06-23.
- "Rickettsia rickettsii: The Cause of Rocky Mountain Spotted Fever". Multiple Organisms: Organismal Biology. University of Wisconsin-La Crosse. 2007.
- "Rocky Mountain Spotted Fever (RMSF)". Centers for Disease Control and Prevention. 21 November 2013.
